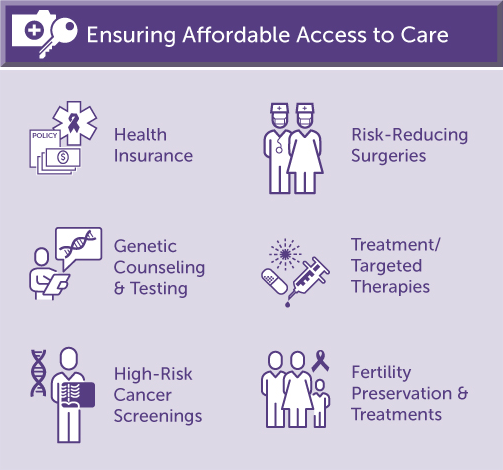
Health Insurance
The Affordable Care Act (ACA) significantly expanded consumer protections and the availability of health insurance and for Americans. The law contains several provisions that benefit members of the hereditary cancer community, banning the practice of charging more or denying health insurance coverage due to a pre-existing health condition such as cancer, prohibiting health plans from putting annual or lifetime dollar limits on most benefits, coverage of certain essential health services and screenings with no copay and more.
FORCE is a proponent of policies that facilitate affordable access to quality health insurance and care for all Americans. We continue to advocate for improvements to the ACA, private and employer sponsored health plans, Medicaid and Medicare.
Genetic Counseling and Testing
The Affordable Care Act requires health insurers to cover genetic counseling and BRCA testing for women who meet certain criteria, with no out-of-pocket costs to the patient.
BRCA genetic testing for men—and women who are currently undergoing cancer treatment—are not covered under the ACA preventive services. Similarly, genetic testing for mutations other than BRCA1 and BRCA2 (i.e. ATM, CHEK2, PALB2, Lynch Syndrome, etc.) is not covered under the ACA. Many health insurers cover the testing but deductibles, coinsurance and copays apply. Medicare only covers genetic testing for an inherited mutation in individuals with a cancer diagnosis who meet certain personal or family cancer history criteria. Most Medicaid programs cover testing for BRCA mutations and some cover testing for Lynch syndrome; eligibility varies by state.
FORCE advocates for coverage of genetic counseling and testing (including multigene panel testing) as appropriate for those diagnosed with cancer as well as unaffected men and women (previvors) who meet National Comprehensive Cancer Network (NCCN) guidelines.
High-Risk Cancer Screenings
Currently, federal law requires health insurers to cover the following with no out-of-pocket costs for the patient:
- annual mammograms for women age of 40 and older
- colonoscopy every 10 years, or other methods of colorectal cancer screening, for people age 45 and older
- cervical cancer screening with a Pap test every 3 years for women ages 21-65
National medical guidelines recommend earlier, more frequent and more intensive screenings for people at an increased risk of cancer due to genetics or other factors. Health insurers are not required to cover high-risk screenings, such as breast MRIs, mammograms before age 40, colonoscopies before age 45 or PSA testing.
Most health insurers cover medically necessary screenings and diagnostic services beyond those legally required, but coverage does not mean 100% payment by the insurance company. Patients may incur significant out-of-pocket costs because deductibles, coinsurance and copays apply.
Medicare generally does not cover the cost of screenings beyond those needed by the “average risk” population. Medicaid coverage of high-risk screenings varies by state. National Breast and Cervical Cancer Early Detection Program (NBCCEDP) funds can be used for annual breast MRIs and mammograms for low-income, uninsured and underserved women who are considered high-risk, but the majority of state NBCCEDP programs only cover screenings needed by those at average risk of breast cancer.
FORCE strongly supports policies that reduce or eliminate the cost of medically necessary screenings and diagnostic tests for those at increased risk of cancer. High-risk individuals should not face exorbitant out-of-pocket expenses for guideline-recommended cancer screenings.
Risk-Reducing Surgeries
Prophylactic or risk-reducing surgery is recommended for certain people at increased risk of cancer. Expert medical guidelines encourage risk-reducing salpingo-oophorectomy or hysterectomy, and consideration of mastectomy for individuals with specific mutations.
Although these surgeries are preventive in nature, insurers rarely cover them in full. Deductibles, coinsurance and copays apply. In some cases, risk-reducing surgery may not be covered at all. Medicare is essentially prohibited from covering risk-reducing surgeries. Medicaid coverage of prophylactic surgeries varies by state.
FORCE advocates for affordable coverage of expert-recommended interventions such as surgery that prevent or reduce the risk of cancer for high-risk individuals. Nobody wants to undergo surgery but limiting the financial impact helps ensure equitable access to these potentially life-saving measures.
Treatment / Targeted Therapies
Even with health insurance, many people encounter significant out-of-pocket expenses when undergoing cancer treatment. This is especially true for patients receiving newer therapies and those administered orally, like PARP inhibitors.
FORCE advocates that patients, with guidance from their providers, should have a choice in the evidence-based treatment they receive. We endorse increasing clinical research on targeted therapies and companion diagnostics to determine who benefits most from these therapies. We also support reducing the cost of treatments regardless of how they are administered, limiting patients’ out-of-pocket costs, and eliminating specialty tiers, step-therapy practices and copay accumulators. A cancer diagnosis is difficult physically and emotionally; we work to minimize financial burden and administrative red tape so patients can focus on their health.
Fertility Preservation and Treatments
Some cancers and cancer treatments affect fertility. This is particularly true for individuals with cancers caused by inherited mutations because these are more likely to be diagnosed at an earlier age, before their family is complete. National guidelines recommend that young people diagnosed with cancer explore fertility preservation prior to starting treatment.
Women with certain inherited genetic mutations are at increased risk of ovarian, endometrial and related gynecologic cancers. Unfortunately, there is no reliable screening or early detection for these cancers so medical guidelines recommend risk-reducing surgery to remove their ovaries, fallopian tubes and/or uterus. Some women wish to undergo fertility preservation before surgery to remove their reproductive organs.
Individuals with an inherited genetic mutation causing increased risk of a disease, such as cancer, may consider Preimplantation Genetic Diagnosis (PGD), a medical procedure that allows people to have children who do not carry the mutation.
Health insurers typically do not cover fertility preservation or related treatments. While several states have passed fertility preservation coverage laws, there is no such coverage in the majority of states.
FORCE supports policies that facilitate affordable access and insurance coverage of fertility preservation for any individual of childbearing age who will experience infertility due to surgery or treatment. We also advocate for coverage of related procedures including in vitro fertilization (IVF) and PGD as desired by these patients.