PUBLISHED: 11th February 2022
by Joel Axler
As a lifelong vegetarian and trailrunner, at 54, I wasn’t expecting to be talking to my doctor about the possibility of prostate cancer. I’m proud of my fitness and healthy lifestyle, and prostate cancer was something I thought you might have to worry about when you’re older. My mildly high PSA was a red flag though, and my family history for the BRCA2 mutation concerned my doctor. I hadn’t been tested for the mutation. As a man, I was unaware of the importance. My doctor ordered the test and the lab soon confirmed that I had the mutation. And so my journey began. A month and a half later, a biopsy at the urologist’s office confirmed that I had Gleason 6, low-risk prostate cancer. The evidence suggested that I was the perfect candidate for Active Surveillance (AS), which requires regular monitoring of certain biomarkers to keep an eye on the progression of the cancer. I wasn’t certain about the impact of my BRCA2 mutation, though. My doctors offered little insight and I struggled to find information relevant to someone my age with similar diagnostic variables.
I sought information from every source I could find to help me understand my diagnosis. One evening I decided to attend an online support group sponsored by AnCan, an organization that provides virtual support for people who live with a serious disease or condition. I intended to remain anonymous and just listen to others but as a new attendee, I was asked to share my story. The experienced volunteer moderators immediately felt it was important for me to connect with leading experts on hereditary risk and prostate cancer. They reached out to experts on my behalf, and the next morning, I had emails from four or five national figures, all with a similar message: early research suggests that AS may not be the best choice for BRCA2 mutation carriers who have low-risk prostate cancer. They further qualified this conclusion by adding that if I chose AS, monitoring should be carried out very carefully_“Super Active Surveillance,” I later heard it called.
I listened, and then I spoke with one of the experts via a telemed consultation. I read the original research. Although prostate cancer is known to grow slowly in most patients, that may not be true in individuals with certain germline mutations, and BRCA2 is particularly concerning. Early research seems to show that prostate cancer can progress swiftly, from “0 to 60” one of the experts said, and it can be difficult to monitor with typical biomarkers like PSA. Research with patients at more advanced stages shows that those with BRCA2 mutations have particularly aggressive prostate cancers. Even the NCCN Guidelines on prostate cancer treatment highlight BRCA2 as a variable that should be considered when deciding on a response.
It was a lot to think about. After my initial diagnosis, I transferred my treatment from my small city to a high-volume, reputable medical center a couple of hours away. My biopsy slides were re-analyzed, and my cancer was re-classified as Gleason 7, intermediate (favorable) risk. I still had all options on the table, my new specialist told me, and he seemed relatively unconcerned about my BRCA2 status. I’ve found doctors to be pretty hesitant about providing direct recommendations, and I’ve agonized over the decision. I finally determined that it was mine alone. I don’t want the harsh consequences of treatment, but I also don’t want to risk the window of curability closing on me. My BRCA2 mutation is a wild card and the evidence of its impact on cancer progression is alarming. I’ve decided to have prostate surgery. Based on all the information I’ve collected and the experiences I’ve been through, it’s the right decision for me. Everyone has their own journey. This is mine.
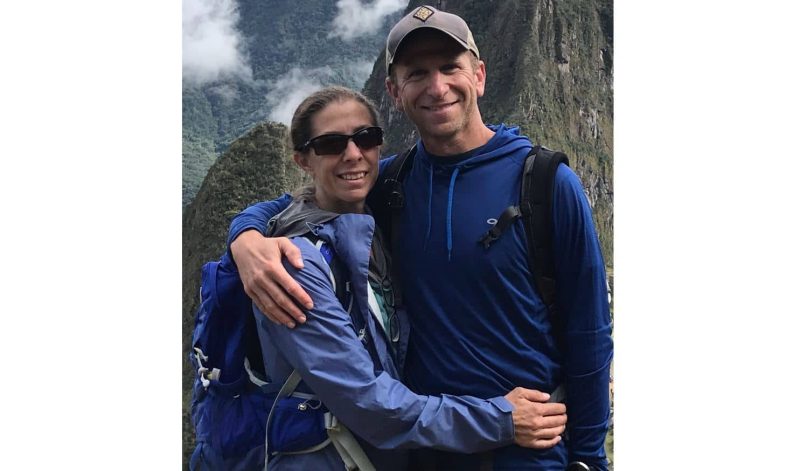
Joel and his supportive wife Randi live in Flagstaff, Arizona where they raised their boys and continue to enjoy high-altitude outdoor pursuits. In between days spent trailrunning, backpacking or hiking. Joel works as a full-time school psychologist.
7 Comments
May 2, 2024
Hi Joel, Wondering how you are doing? Recently found out im BRCA2 positive and trying to get a grip of it all. thanks
Michael Di Monaco
Reply
October 8, 2024
Hi Michael, I’m doing well. 2.5 years later and PSA is still undetectable. I check it every 4 months right now. Surgery like that isn’t without consequences but am still satisfied overall. Joel
Joel
Reply
May 2, 2024
Hello Joel, just wanted to know how you are doing. Found out im BRCA2 positive, and trying to get a grip of it all. thanks
Michael Di Monaco
Reply
August 1, 2022
Thanks for sharing.
Marie Blain
Reply
April 28, 2023
Dear Joel Thanks for sharing. I wonder if I might ask you to reflect on a matter, that is weighing greatly on myself these days. I am BRCA2 positive and a mother of several boys. I couldn’t help noticing that you yourself have boys and that you are a school psychologist. My question is this. When did you tell your children about their possible risk of carrying the BRCA mutation? And how does one go about this stuff without freaking them out. My boys are still very young but I spend a great deal of late hours thinking about this. All the best
Nenna
Reply
December 6, 2023
Hi Nenna, Sorry for the late reply but I didn't notice the comment. My boys were young adults when I found out so I simply had a direct conversation with them. With younger children, I think you have the benefit of time. That is, you can begin having discussions about these things at different times, at developmentally appropriate levels. You could for example, simply introduce the concept of genes and how they influence things like our hair color. As kids get older you can continue the conversation by pointing out that genes influence our health. I don't think it's important to personalize it while they're young until it's necessary. For example, if a parent is undergoing a treatment that may need to be explained. FORCE has a booklet addressing the issue of discussing mutations with children and it's pretty helpful. You may need to Google it to locate it. Best wishes in your journey. Joel
Joel
Reply
November 2, 2022
UPDATE: I had my surgery as planned and am about 7 month post and doing fairly well. My post-surgical pathology uncovered a Gleason 9 tumor, extra-capsular extension, and invasion of the seminal vesicles. None of that was known before surgery. No lymph node involvement though so I’m on the planned every 3 month PSA check to monitor for recurrence. So far so good. There’s no way to know for sure if my much more aggressive prostate cancer is directly related to my BRCA2 status, but my pre-surgery notion of BRCA2 as a wild card seems to hold true. I’m satisfied with my treatment decision and can only imagine my situation had I not made it. (I’m not endorsing any treatment option and strongly encourage men to find the highest quality treatment center, do their own research using reputable sources, and make decisions based on their own unique situation.)
Joel
Reply