PUBLISHED: 17th November 2022

Tips to keep your skin comfortable and prevent skin infections from a dermatologist-turned-cancer patient.
Preventing skin infections and easing skin side effects during chemotherapy help to support your health and comfort during treatment. As a dermatologist, I know that every cancer patient benefits from knowing how to take good care of their skin because all breaks in your skin during chemo are at risk for infection. This includes breaks in your skin from wounds and rashes. Wounds can be accidental or surgical. Skin rashes during chemotherapy are also common. They happen randomly as they do in non-cancer patients but cancer treatment puts us at increased risk due to allergic reactions to the many medicines we are given, surgical tape used to dress our wounds and other aspects of our cancer care.
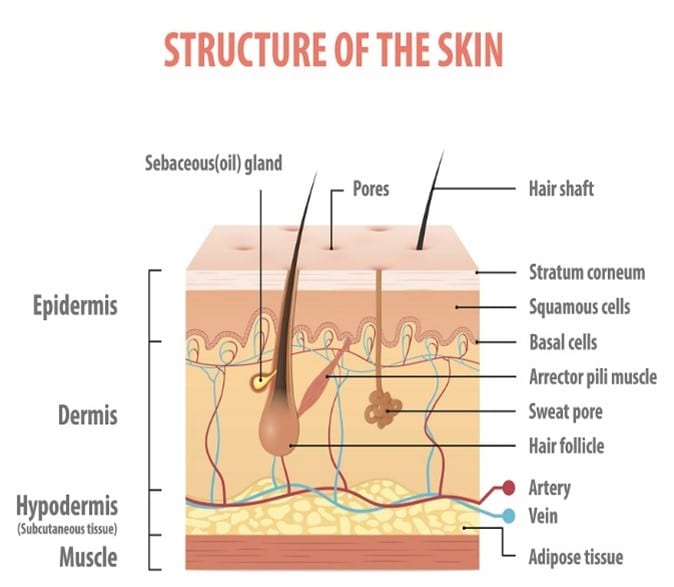
To put the importance of this subject in context, your skin is your body’s biggest organ, and it’s your trusted protective coating from germs in the outside world. Before becoming a cancer patient, we all experience wounds and rashes that heal without difficulty. During chemo, however, our ability to heal and fight infection is altered. Wounds and rashes may not heal well and our immune system may not be able to prevent simple skin breaks from becoming infected. Skin infections may impact our cancer treatment, resulting in antibiotic treatment and even delays in our chemotherapy treatment schedule.
The bottom line is that keeping our skin healthy and preventing skin infections during cancer treatment is an important step we can take to ease our treatment process
As a dermatologist, I had the advantage of understanding what I needed to do to keep my skin healthy and fend off side effects during my treatment for aggressive BRCA breast cancer. I took steps to prevent some of the common and preventable skin problems that are inherent in being a chemo patient. I also used topical treatment to prevent small wounds from becoming infected. I’m going to share this info with you in the hope that it will help you keep your skin healthy, comfortable and free from problems during your cancer treatment.
Every cancer patient faces universal skin challenges during treatment, including:
- Your skin will be drier, more sensitive and more fragile than ever before. Dry skin will itch, can be uncomfortable and prone to eczema, with resulting scratch wounds and sores. Skin peeling and blisters on the hands and feet are also side effects of many of the chemo drugs used during our treatments.
- Dry hands and irritant hand dermatitis are a risk due to frequent hand washing and the use of hand sanitizers that we depend on throughout the day to fight infections—especially when we are in medical facilities where the presence of super germs is more common.
- Allergic reactions and sun sensitivity can occur from the many drugs we receive during our cancer treatment. This may cause allergic rashes and excessive sunburns that create skin injury.
- Nails and cuticles can become brittle during chemo and some chemo medicines may even cause nail deformity and lifting, which can make nails fragile, painful and prone to injury.
- Immune suppression from chemotherapy gives germs a unique advantage during treatment and puts us at increased risk of infection.
The good news is that simple changes in our skin care routine can help us avoid problems and keep our skin healthy.
Skin care tips for chemotherapy
Tip #1: Use a hydrating gentle skin care routine daily. The key to a simple health-promoting skin care routine during chemo is to use gentle hypoallergenic skin cleansers followed by deeply hydrating hypoallergenic moisturizers every day. Avoid unnecessary allergens (such as fragrance) and irritants (such as many acne and anti-aging ingredients). Keep skin care simple and hydrating to maintain comfortable skin during chemotherapy. This in turn helps to fend off skin dryness, which will reduce skin fragility.
- Use only gentle skin cleansers. Cleanse with a gentle pH-balanced cleanser that is free from fragrance and exfoliating ingredients. My favorite options come from the VaniCream line. I like their bar soap, which can be used from head to toe. Other good options include Cetaphil and Aquanil liquid cleansers. Natural soap options have an alkaline pH that is inherent in the soap-making process, called saponification. Select products without botanical essences can be allergens: Yes, they are natural but they have allergens nonetheless, just like poison oak and poison ivy.
- Always rinse well after using a skin soap or cleanser. This is critical to protect the lipids and protein that make up your fragile skin barrier layer. Retained soap or cleanser residue will continue to remove lipids and eventually damage keratin protein if you don’t rinse it off. Pay particular attention to your hands, including the skin under your rings and between your fingers. These are places where irritant hand dermatitis often starts. Take the time to rinse your skin well after every washing.
- Avoid very hot water for skin cleansing. The water temperature for your skin cleansing should be warm but not steamy hot. Remember that hot water rinses grease and grime off pots and pans better than cooler temperatures. You don’t want that efficiency with skin cleansing because it equates to the loss of intercellular lipids in your skin’s barrier layer.
- Always apply moisturizer within 3 minutes after toweling skin dry following cleansing. Moisturizer traps water that your skin just absorbed during cleansing. Apply a rich moisturizer with occlusive ingredients such as hypoallergenic botanical oils, petroleum jelly, mineral oil or dimethicone. Other widely available water-binding ingredients in moisturizers include glycerin and hyaluronic acid. Finger or toe fissures can be treated with a more occlusive ointment such as Aquaphor or Bag Balm and covered with therapeutic cotton gloves.
- Avoid moisturizers with fragrance-and allergen-and irritating ingredients, including some of the anti-aging and acne ingredients such as salicylic acids, glycolic acid (AHAs) and retinol. These latter ingredients exfoliate precious skin barrier cells that are reduced during chemo. It’s fine to apply moisturizer to the skin between washings but it’s not nearly as hydrating for your skin as when you apply it after your skin has been washed.
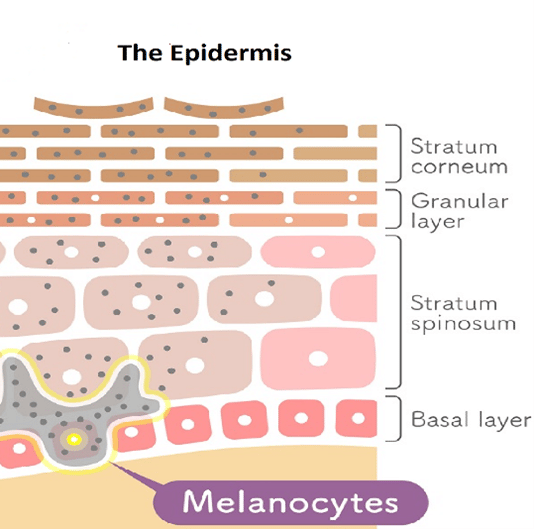
Like a trip to the dermatologist, this hydrating gentle skin care routine is the same advice we would give you to help heal many types of skin problems such as a rash from a medication allergy, peeling fingers or toes from chemotherapy medicines, chapped skin from harsh weather, etc. This is a skin care routine that helps heal any disruption in your skin’s epidermal barrier. The epidermal barrier is composed of keratin protein-filled living cells that transition to dead cells in the stratum corneum (the outer layer of the epidermis).
Throughout the epidermis, these cells are mortared together by lipids. The epidermis compromises your skin’s important barrier layer that protects you. Your skin care routine is a key self-care step that helps you to maintain a healthy epidermis and heal rashes.
Using myself as a living laboratory, I created a simple Chemotherapy Skin Care Kit with the products I used to care for my skin during my year of cancer treatment. Your dermatologist may also prescribe a medicine to speed healing, but we use the medicine in addition to these gentle hydrating skin care principles.
Tip #2: Protect your skin daily from the sun to prevent photoallergic drug reactions. Many medicines are capable of causing a rash or burn when your skin is exposed to UV rays. It’s called drug-induced photosensitivity. Photosensitizing medicines include some common antibiotics, chemotherapy drugs, antihistamines, nonsteroidal anti-inflammatory medicines, high blood pressure drugs and diabetes drugs, just to name a few. During cancer treatment, you may be on a lot of medicines—both the medicines used specifically to treat cancer and other medications to help your body tolerate those medicines. Surgical procedures, and even some of the tests used to evaluate our treatment progress, expose us to more medicines. The bottom line is that during cancer treatment, we are given a lot of medicines, some of which will be photosensitizers. Sun protection lowers the risk of a photosensitive reaction.
- Cover as much of your exposed skin with clothing made of UPF 50 or a thick-weave fabric. Wear a mineral zinc oxide broad spectrum SPF 30 or higher sunscreen on uncovered skin. Get into the habit of applying sunscreen in the morning to uncovered skin and reapplying during prolonged sun exposure. Remember that UV rays bounce into the shade from reflected surfaces and can come through window glass.
Tip #3: Use good wound care to treat all superficial skin injuries during chemo. In my dermatology practice, I’ve made—and treated—wounds for years. Yep, it's part of my job and expertise so I'm very familiar with wound care and how to reduce the risk of skin infection. For all skin wounds, I instruct my patients to apply a Vaseline-type ointment and cover the wound with a bandage, changing the dressing and ointment daily until the wound is healed. When I’m concerned that a wound may become superficially infected, I prescribe mupirocin ointment and have patients use that in place of Vaseline under their bandage three times a day. Mupirocin also provides the occlusive Vaseline-type of ointment base that helps to heal wounds. Mupirocin Ointment is a prescription medication and it’s important to ask your treatment team if this medicine is appropriate for your care.
While receiving chemotherapy, I decided that all my skin wounds would benefit from this extra precaution and that’s how I treated them. It worked beautifully and I know for a fact that two wounds I developed would have required oral antibiotics were it not for this simple and preventative wound care routine that turned them around and allowed them to heal. Our skin is our largest organ, protecting us from germs, allergens and irritating substances. During chemotherapy, skin cell turnover is reduced and our skin is drier and more fragile than before treatment; exposure to allergens and irritants in skin care products or harsh chemicals penetrates more readily and skin moisture is lost faster. Germs also pose a greater threat and medicines can have skin side effects. By strengthening our skin barrier with hydrating gentle skin care, protecting our skin from UV rays, and treating all skin wounds promptly, we can reduce our risk of skin problems during our cancer treatment. I’m grateful that this strategy worked for me during cancer treatment, and I hope that it helps to prevent any serious skin problems during your cancer treatment.

Cynthia Bailey, M.D. is a board-certified dermatologist who has practiced for over 30 years in California. In 2013, Dr. Bailey was diagnosed with bilateral high-grade triple-negative breast cancer. She is a breast cancer survivor, ovarian cancer previvor and BRCA1 mutation carrier. She is also the Founder of DrBaileySkinCare.com
References:
Saadet, ED and Tek I. Evaluation of chemotherapy-induced cutaneous side effects in cancer patients. International Journal of Dermatology 2022.
Fabbrocini G, Cameli N, Romano MC, et al. Chemotherapy and skin reactions. Journal of Experimental & Clinical Cancer Research 2012;31(1):50.
Biswal SG and Mehta RD. Cutaneous Adverse Reactions of Chemotherapy in Cancer Patients: A Clinicoepidemiological Study. Indian Journal of Dermatology 2018;63(1):41-46.
Deutsch A, Leboeuf NR, Lacouture ME, et al.Dermatologic Adverse Events of Systemic Anticancer Therapies: Cytotoxic Chemotherapy, Targeted Therapy, and Immunotherapy, American Society of Clinical Oncology Educational Book 2020:40, 485-500.
Miller KK, Gorcey L, McLellan BN. Chemotherapy-induced hand-foot syndrome and nail changes: a review of clinical presentation, etiology, pathogenesis, and management. Journal of the American Academy of Dermatology 2014;71:787-94.
Miller KK, Gorcey L, McLellan BN. Chemotherapy-induced hand-foot syndrome and nail changes: a review of clinical presentation, etiology, pathogenesis, and management. Journal of the American Academy of Dermatology 2014; 71(4):787-794.
Hofmann GA and Weber B. Drug-induced photosensitivity: culprit drugs, potential mechanisms and clinical consequences. Journal der Deutschen Dermatologischen Gesellschaft 2021;19(1):19-29.
2 Comments
January 2, 2024
I have been researching all kinds of moisturizers that are best to use during chemo. Your article was very helpful, as now I know what is actually good to use. And your recommended creams don’t cost a fortune. Thank you for sharing your knowledge. I hope you had a good outcome from your treatments.
JoAnne
Reply
September 23, 2023
Great and helpful article!
Susannah Baker
Reply