PUBLISHED: 12th August 2024

A new survey of healthcare providers, policy, and advocacy organizations conducted by FORCE and Living Beyond Breast Cancer in partnership with the National LGBT+ Cancer Network identified improving gender and sexual orientation inclusivity as a priority in providing competent care.
Every patient should have high-quality health care that meets their needs. Many health issues are related to gender or are impacted by gender—everything from cancer screenings, drug prescriptions, and health recommendations for diet or heart health to the impact of hormonal status on treatment plans (1-8).
Clear communication between patient and provider is needed to ensure appropriate care. Healthcare is best when patients can effectively talk and be heard by their provider and feel safe disclosing relevant details that may impact their situation (9-11). Unfortunately, we know that many people, especially LGBTQIA+ people, don’t have access to high-quality care or feel safe disclosing relevant details with their providers (12-14). Guidance for providers on best practices for cancer care for gender-diverse patients is sparse but emerging (15-18).
To improve the quality of care and quality of life of LGBTQIA+ people impacted by cancer, Facing Our Risk of Cancer Empowered (FORCE) and Living Beyond Breast Cancer (LBBC) conducted a survey of healthcare provider, policy, and advocacy organizations to learn about respondents’ preparedness to serve gender and orientation minorities, as well as their needs for training to serve these priority populations. See link for detailed Gender Inclusion survey results. A total of 153 people representing organizations that serve people with breast cancer, including hospitals and healthcare provider, non-profit or advocacy organizations, and public health agencies, responded to the survey from March to September 2023. The complete survey illustrates that there is much work to do to ensure every person facing a breast cancer diagnosis gets the care they need—and deserve.

.
Collection and use of pronouns and other gender information is uneven
Pronouns represent how people self-identify. Using an individual’s indicated pronouns shows respect and validation of lived experiences. Failure to use indicted pronouns signals a general disrespect and may be alienating, disrupt communication, and create a barrier to appropriate healthcare. Asking about pronouns is the first step in appropriately addressing patients. Depending on outward appearance, voice or names can be misleading, regardless of a person’s gender.
Most (80-99 percent) of respondents said they are at least somewhat familiar with terms, such as assigned sex at birth, cisgender, gender, genderfluid, genderqueer, non-binary, and transgender. The majority were familiar with all except two-spirited, a term used by some indigenous populations (41% were very or somewhat familiar). However, in addition to two-spirit, genderfluid, genderqueer, and cisgender were less familiar to 15-20 percent of respondents.
Still, a minority of organizations consistently collect information on pronouns or other gender information. On the upside, nearly half of the organizations that do collect pronouns at least some of the time also ask for additional information about gender, such as sex assigned at birth.
Organizations collected pronouns or other gender information in a variety of overlapping ways:
- 75% by electronic records
- 27% during appointments
- 26% via patient portals
- 10% via support or navigation forms
- 8% via feedback surveys
Only 29% of respondents said their organizations have a policy about using pronouns.
.
Use of visual signs of welcome varied widely
Visual signs signal to patients that a healthcare setting is a safe and welcoming place. What is meant by a visual sign of welcome? Language and images that include a diverse representation of gender:

- including gender-neutral or inclusive signage
- gender-neutral or inclusive restrooms
- Patient information depicting a variety of genders or specifically geared toward the LGBTQ+ community
- Staff badges indicating pronouns or other signs of inclusion for the LGBTQ+ community
- Posted non-discrimination statements or patient bill of rights, including sexual orientation/gender identity
- Online accessible information about being a safe space for people of all sexual orientations/gender identities
Best practices for places of healthcare include all of these signs of welcome.
Our survey found that many surveyed organizations use one or more of the signs of welcome but few/none used all of them. Nearly half of organizations posted non-discrimination statements, information online about being a safe space for all, and inclusive patient education materials. However, only one-third used pronouns on staff badges, gender-neutral or inclusive signage, hospital gowns, and restrooms. Many respondents were unsure about whether their organizations offer each sign of welcome, indicating lack of organization-wide awareness and engagement.
Use of visual signs of welcome is an internal change within an organization that could have a substantial impact. Letting people know they are in a welcoming space can facilitate more open communication and patient sharing of key health information with their providers. This is important for successful healthcare.
.
Patient materials lack gender inclusivity
Patient documents and educational materials should be written in a way that does not discriminate against a particular sex or gender, does not perpetuate gender stereotypes, and improves communication with patients. For example, avoiding the terms “men” and “women” when “people at risk for breast cancer” could be used.
This can also help convey that everyone can get breast cancer—although at different frequencies—an often misunderstood fact (19-20). For those assigned female at birth, the lifetime breast cancer rate in the general population is 13% but can be up to 70% among people with certain inherited mutations. Among people assigned male at birth, the lifetime risk of breast cancer is 0.1% but rises to 7% among those with certain inherited mutations. Mastectomy can reduce those risks and is sometimes recommended for people at high risk due to certain inherited mutations. For those considering gender-affirming surgeries, it is important to discuss personal or family cancer history, as gender-affirming top surgery may not be as complete as risk-reducing mastectomy recommended to reduce hereditary cancer risk (21).
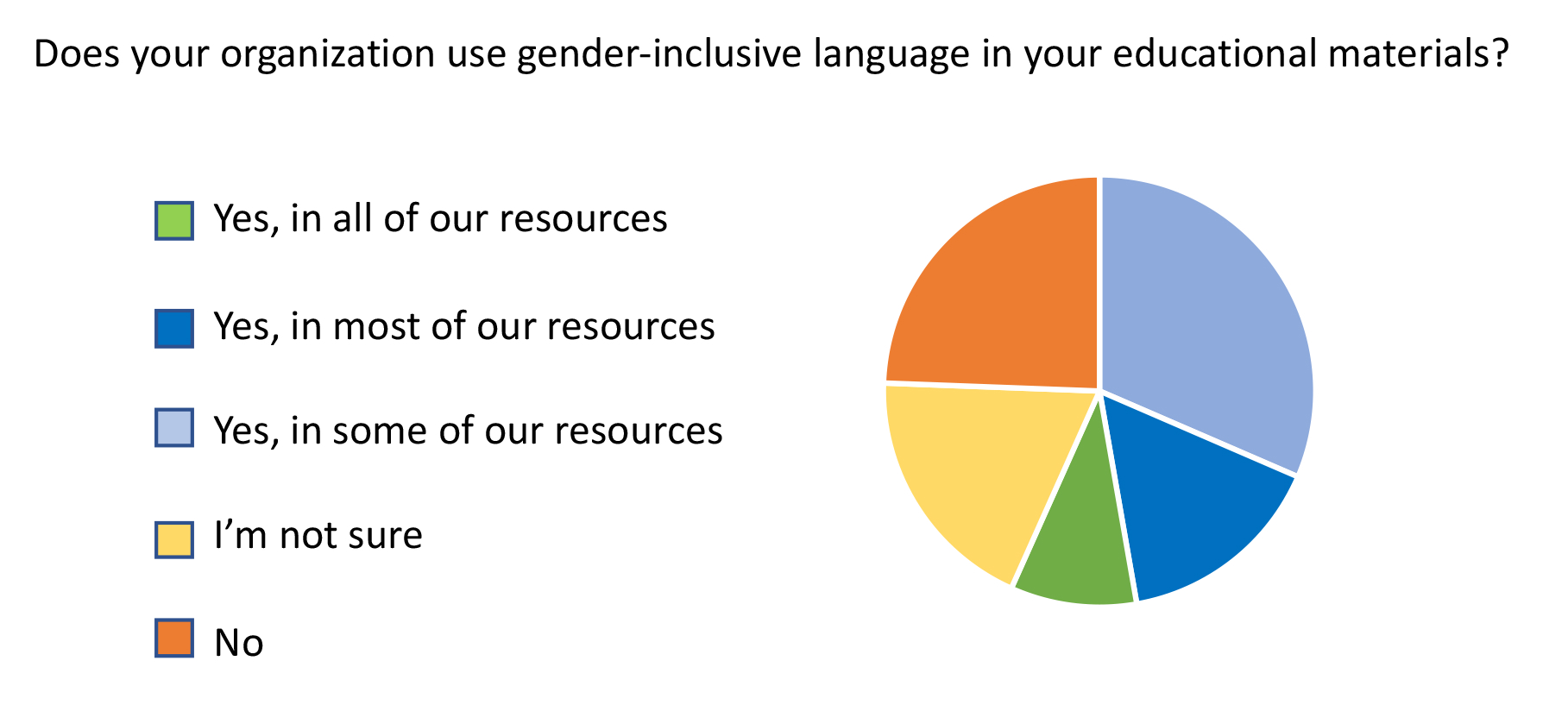
When it comes to putting gender-inclusive language into practice, only 9% of respondents' organizations used it in all patient education materials, 47% sometimes or mostly did, 24% didn’t, and 19% were unsure. However, that appears to be changing. Seventy-nine percent of respondents indicated that their organizations were moving toward more gender inclusive language and 51% indicated that these issues were of high or very high priority in their organization. However, 22% indicated these issues were a low or very low priority for their organization and 29% were unsure of their organization's priority.
Among respondents, some organizations had or were in the process of implementing The National Academies of Science, Engineering, and Medicine (NASEM) recommendations on data collection of sex, gender identity, and sexual orientation. However, the vast majority were unsure whether these recommendations were being considered.
.
Gender and breast cancer screening
Use of gender-inclusive language is a good first step to providing inclusive care. It is also important to consider patient education for all populations to ensure patients have the information needed to adhere to recommended cancer screening, identify cancer signs, and get prompt cancer diagnoses. Finding and treating cancer early improves survival outcomes and quality of life for cancer patients.

In the case of breast cancer screening, this requires personalizing screening information for specific patients.
For example, screening all people assigned female at birth (AFAB) for breast cancer, consistent with guidelines, is important. But there are specific considerations for trans men, including:
- surgical considerations
- inherited mutations and risk
- gender-affirming hormone considerations
While some trans men have top surgery, which reduces their risk of breast cancer, this surgery differs from the more extensive bilateral mastectomy recommended as a risk-reducing measure for those at high risk due to an inherited mutation. Discussions between providers and patients about these issues and representation in patient materials are key to assuring that patients have the information they need to make informed decisions about their preventive care.
A major issue for patients assigned male at birth (AMAB) is providing appropriate breast cancer screening for those who are at high risk. This was noted by several survey respondents. While the frequency of breast cancer among those AMAB is low (0.1% in the general population), it can be as high as 1-7% among those who have an inherited mutation in a gene that increases breast cancer risk. This is important for all people but particularly for trans women whose care may be overlooked in this regard.
Additionally, there is little information about the impact of gender-affirming hormonal care on breast, endometrial, ovarian, and prostate cancer risk. Highlighting information that is available is important: for example, guidelines from the American College of Radiology for breast cancer screening for transgender women/trans femme folks who are on HRT. Furthermore, it is important that providers do not make assumptions about gender that could lead to underscreening and underdiagnosis of cancer or other health issues.
.
Barriers to collecting gender data and implementing gender-inclusive language
When asked about barriers to collecting gender data and implementing gender-inclusive language, the most common response was a lack of certainty about whether barriers existed or not. This lack of certainty suggests a lack of cohesive, organization-wide planning regarding gender inclusivity issues.
Of those who responded to whether there were barriers to implementation of gender-inclusive language at their organization, 34% reported barriers, including:
- lack of awareness of the importance of inclusive language
- resistance of staff, leadership, or physicians
- cost of updating existing materials
- lack of time
- religious objections
- lack of commitment or communication about the use of inclusive language
- political pressure
- lack of research data on sexual orientation and gender minority groups to include in informational materials
- difficulty achieving consensus on terminology
- difficulty translating gender-neutral terms into Spanish
Of the barriers cited, lack of awareness of the importance of inclusive language was the most commonly reported. To counter this barrier, most indicated a need for general information about why gender inclusivity is important and why language specifically is important. Other suggested supports included:
- materials to engage staff
- lists of appropriate terms to use
- examples of materials with inclusive language
- training materials
- information about NASEM and other guidelines for collecting information and examples of templates for data collection
- examples of Spanish language materials
.
Tips for creating more inclusive environments
Avoid assumptions and stereotypes
- Strive for respectful and accurate engagement with patients. Avoid generalizations and default assumptions as these may create barriers to effective healthcare. Treat each person as an individual with unique healthcare needs. Do not assume that a given person will want or not want particular tests, diagnostics, or information.
Replace outdated labels with appropriate wording: pronouns and gender identity
- Keep current on terms in your field. Be aware that language is constantly shifting and evolving. Using preferred language/terms shows respect. Asking for and using the pronouns that person indicates as well as terms that reflect their gender identity is common courtesy and better builds provider-patient interactions.
Use inclusive language
- Using language that focuses on the healthcare issue in question can improve communication with patients.
- The terms "people," "individuals," or "patients" can often be used rather than "men and women."
- For more gender-driven topics, an organ-based approach is often more accurate and less confusing. For example, "People with a uterus should be aware of the signs of endometrial cancer" is more inclusive than "women should be aware of the signs of endometrial cancer." The former includes transgender people with a uterus and excludes people who have had a hysterectomy, focusing the message on the appropriate audience.
Create welcoming, inclusive physical spaces, including signage and symbols
- Have imagery in facilities that reflect patient diversity to show inclusion.
- Have gender-neutral or inclusive restrooms with clear signage, e.g., convert single-use person restrooms previously signed for men and women to all genders.
- Have patient information depicting a variety of genders or specifically geared toward the LGBTQ+ community.
- Have staff badges indicating pronouns or other signs of inclusion for the LGBTQ+ community.
- Post non-discrimination statements or a patient bill of rights, including sexual orientation/gender identity.
- Communicate online about being a safe space for people of all sexual orientations/gender identities.
Use communication methods that support gender inclusion
- Update patient materials to incorporate inclusive language, imagery, and approaches.
- Use patient-indicated pronouns, gender identification, and name preferences consistently across staff. Overlooking or dismissing patients' preferences can undermine and reduce communication and lead to suboptimal healthcare.
- Support inclusion by making practices mainstream and standard in both written and spoken communications.
- Make sure new staff and students/interns are updated appropriately.
Ensure healthcare research is inclusive
- Lack of information about LGBTQIA+ groups hinders healthcare. When doing healthcare research, inclusion is essential in both the study design process and participant recruitment to address gaps in knowledge and build evidence-based recommendations.
Incorporate training about LGBTQIA+ patients in continuing education
- Education about patient needs and inclusion is an ongoing process. Include gender diversity training with other continuing education or professional development to regularly address changing issues. Encourage colleagues to participate and departments to include inclusion training as a regular part of their education process.
Build individual and institutional commitments
- Listen to lived experiences of the gender-diverse community. Create policies and protocols to standardize inclusive practices in your institution/organization. As materials are updated, make sure that they are reviewed for inclusion and cultural sensitivity. Ask members of the LGBTQIA+ community to participate in the creation of research study designs.
(Adapted from Marjadi B and colleagues' paper: Twelve Tips for Inclusive Practice in Healthcare Settings. Int J Environ Res Public Health. 2023 Mar 6;20(5):4657.)
You can create a foundation for gender-inclusive spaces by incorporating simple steps over time, such as learning more LGBTQ+ vocabulary, using gender-neutral language and pronouns, and participating in training and workshops.
.
Resources
- FORCE/LBBC: Gender inclusion survey of healthcare organizations
- FORCE XRAY reviews: LGBTQIA+ issues
- FORCE blogs: Transgender issues
- FORCE XRAY review: Breast cancer risk for transgender women with inherited mutations
- FORCE XRAY review: Breast cancer risk for transgender men with inherited mutations
- LBBC: LGBTQ+ with breast cancer
- LBBC: Keys to inclusive and safe care for the LGBTQIA+ breast cancer community
- LBBC Resource Guide: Resources for the LGBTQIA+ breast cancer community
- LBBC: Breast cancer and transgender people
- LBBC: LGBTQIA+ and breast cancer care: A guide for providers
- NCCN: NCCN Language Guidance: Sensitive, Respectful, and Inclusive Language for NCCN Publications
- NCCN: Advancing Health Equity for LGBTQ+ Identifying Patients with Cancer infographics supporting more gender-inclusive care for cancer patients
- NCCN: Guidelines for Breast, ovarian, uterine, and prostate cancer risk reduction strategies for transgender, non-binary, and gender diverse people with hereditary cancer syndromes (pg. TNBGD-1)
- National LGBT Cancer Network offers many resources including training on creating welcoming spaces and a searchable list of providers highlighted below.
- Welcoming Spaces: Treating Your LGBTQ+ Patient: Created in collaboration with the Society for Gynecologic Oncology, this training relays best practices for healthcare providers.
- Searchable LGBTQ-welcoming provider lists
- Marjadi B, et al. Twelve Tips for Inclusive Practice in Healthcare Settings. Int J Environ Res Public Health. 2023. Mar 6;20(5):4657.
- Safe Zone Training: Free online resources for training staff on gender inclusion issues.
References
1. Ward BW, et al. Sexual orientation and health among U.S. adults: National Health Interview Survey, 2013. 2014. National health statistics reports; no 77. Hyattsville, MD: National Center for Health Statistics.
2. Dickstein DR, et al. Sexual health and treatment-related sexual dysfunction in sexual and gender minorities with prostate cancer. 2023. Nat Rev Urol. 20(6):332-355.
3. Chen MH and Epstein SF. Tailored to a Woman's Heart: Gender Cardio-Oncology Across the Lifespan. 2023. Curr Cardiol Rep. 25(11):1461-1474.
4. Mehta TS, et al. Cultural Competence in the Care of LGBTQ+ Patients: A Primer for Breast/Chest Centers. 2023. J Breast Imaging. 5(4):473-479.
5. Chowdhury A, et al. Review of Breast Imaging in Transgender and Gender-Diverse Patients: Gender-Affirming Care, Histopathologic Findings, Breast Cancer Risk, and Screening Recommendations. 2024. J Breast Imaging. 6(3):238-245.
6. Ahrendt H, et al. Multidisciplinary management of sexual and gender minorities with bladder cancer. 2024. Urol Oncol. S1078-1439(24)00496-4.
7. Wojcik R and Morris A. Aiming to Improve Equity in Lung Health: Sex and Gender. 2023. Clin Chest Med. 44(3):613-622.
8. Smart AC, et al. Gender-Affirming Surgery and Cancer: Considerations for Radiation Oncologists for Pelvic Radiation in Transfeminine Patients. 2023. Int J Radiat Oncol Biol Phys. 117(2):301-311.
9. King A and Hoppe RB. "Best practice" for patient-centered communication: a narrative review. 2013. J Grad Med Educ. 5(3):385-93.
10. Littell RD, et al. Advanced communication: A critical component of high quality gynecologic cancer care: A Society of Gynecologic Oncology evidence based review and guide. 2019. Gynecol Oncol. 155(1):161-169.
11. Dennison Himmelfarb CR, et al. Shared decision-making and cardiovascular health: A scientific statement from the American Heart Association. 2023. Circulation. 148(11):912-931.
12. Patterson CJ and Sepulveda M-J, White J, eds. Understanding the Well-Being of LGBTQI+ Populations. Consensus Study Report. Washington, DC: The National Academies Press, 2020, p. 436.
13. Cathcart-Rake EJ. Cancer in sexual and gender minority patients: Are we addressing their needs? 2018. Current Oncology Reports, 20(11), 85.
14. Haviland KS, et al. Barriers and facilitators to cancer screening among LGBTQ individuals with cancer. 2020. Oncology Nursing Forum, 47(1), 44–55.
15. Griggs J, Maingi S, Blinder V, et al. American Society of Clinical Oncology position statement: Strategies for reducing cancer health disparities among sexual and gender minority populations. 2017. Journal of Clinical Oncology. 35(19):2203–2208.
16. Sterling J, et al. Cancer screening for transgender individuals: Guidelines, best practices, and a proposed care model. 2023. Urol Clin North Am. 50(4):563-576.
17. Hodan R, et al. Cancer surveillance for transgender and gender diverse patients with Lynch syndrome: a practice resource of the Collaborative Group of the Americas on Inherited Gastrointestinal Cancer. 2023. Fam Cancer. 22(4):437-448.
18. Lund EM, Burgess CM. Sexual and gender minority health care disparities: Barriers to care and strategies to bridge the gap. Prim Care. 2021;48(2):179–189.
19. NCI SEER cancer statistics.
20. FORCE information: Hereditary cancer and genetic testing: BRCA2 risks
21. FORCE information: Breast cancer risk for transgender men with inherited mutations
22. National Academies of Sciences, Engineering, and Medicine. 2022. Measuring Sex, Gender Identity, and Sexual Orientation. Washington, DC: The National Academies Press.
This project was supported by the Cooperative Agreement Numbers, NU58DP006677 (to FORCE) and 1 U58DP006672 (to LBBC), funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services.