Study: Skin cancer among women with an inherited BRCA mutation
Women with an inherited BRCA1 and BRCA2 mutation have an increased risk of various cancers. Study results suggest that although the risk of non-melanoma skin cancer in these women is similar to the risk of the general population, the risk of melanoma skin cancer is slightly increased. (Posted 7/25/24)
Este artículo está disponible en español.

RELEVANCE
Most relevant for: People with an inherited BRCA mutation.
It may also be relevant for:
- previvors
- people with a genetic mutation linked to cancer risk
- people with a family history of cancer


Relevance: Medium-High


Strength of Science: Medium


Research Timeline: Human Research
What is this study about?
In the general population, risk factors for skin cancer include the amount of sun exposure, fair skin, lighter eye color and a family history of skin cancer.
Inherited mutations in several genes have been shown to increase the risk of skin cancer. However, it is unclear if an inherited or mutation increases the risk of skin cancer.
What is this study about?
Researchers of this study wanted to know if having a or mutation increases risk of skin cancer and melanoma.
Why is this study important?
Women who have an in or have an increased risk of several cancers, including breast, ovarian, , peritoneal and pancreatic cancers. However, research on whether having a mutation increases the risk of skin cancer, specifically melanoma, has been conflicting. Because of this uncertainty, people with inherited mutations question when and how often they should be screened for skin cancer.
Study findings
Researchers followed 6,207 women with an in (3,623) or (2,584). The average age of participants was 55. All participants lived in North America (in the United States or Canada).
Women were followed for an average of eight years. The average age at follow-up was 55.
- 232 women reported a diagnosis of any skin cancer.
- 133 had a mutation.
- 99 had a mutation.
- In this study, the lifetime risk of any skin cancer was:
- 14.1% for mutation carriers.
- 10.7% for mutation carriers.
These risks are similar to the lifetime risk of any skin cancer among women in the general population.
- 44 women reported a diagnosis of melanoma.
- 23 had a mutation.
- 21 had a mutation.
- In this study, the lifetime risk of melanoma was:
- 2.5% for mutation carriers.
- 2.3% for mutation carriers.
The lifetime risk of melanoma among or mutation carriers was slightly higher than the lifetime risk in the general population. The risk is 1.5 percent in the general population compared to 2.5 percent for women with a mutation and 2.3 percent for women with a mutation.
Lifetime risk of skin cancer
| Any skin cancer | Melanoma | |
| US women | up to 20% | 1.5% |
| 14.1% | 2.5% | |
| 10.7% | 2.3% |
Skin cancer rates increase with age. In this study, skin cancer rates were highest after age 70.
When researchers looked at previous cancers among participants, the lifetime risk of any skin cancer increased after a breast cancer diagnosis only among mutation carriers.
Other skin cancer genes
The table below lists genes that are linked to an increased skin cancer risk.
| Skin cancer type or syndrome | Genes |
| Melanoma | ACD, *, , BAP1, , CDNK2A, MITF, MC1R , POT1, , RB1, TERF2IP, TERT, , Xeroderma pigmentosa genes |
| BAP1, MBD4, * | |
| Sebaceous | , , , , |
| Basal Cell Carcinoma, including Nevoid Basal Cell Syndrome or Gorlin syndrome | PTCH1, PTCH2, SUFU |
| *More research is needed to confirm a link between a mutation in this gene and increased risk for melanoma. | |
What does this mean for me?
The increased lifetime risk of melanoma among and mutation carriers is slightly higher than the risk of individuals who are not or mutation carriers. Currently, the National Comprehensive Cancer Network (NCCN) does not offer specific screening guidelines for melanoma for people with an in or . However, some experts recommend general melanoma risk management, such as a yearly full-body skin exam, a yearly eye exam (melanoma can occur in the eye) and avoiding too much sun exposure. During a skin cancer screening, show your doctors any suspicious moles or areas of your skin that look concerning or have changed color or appearance.
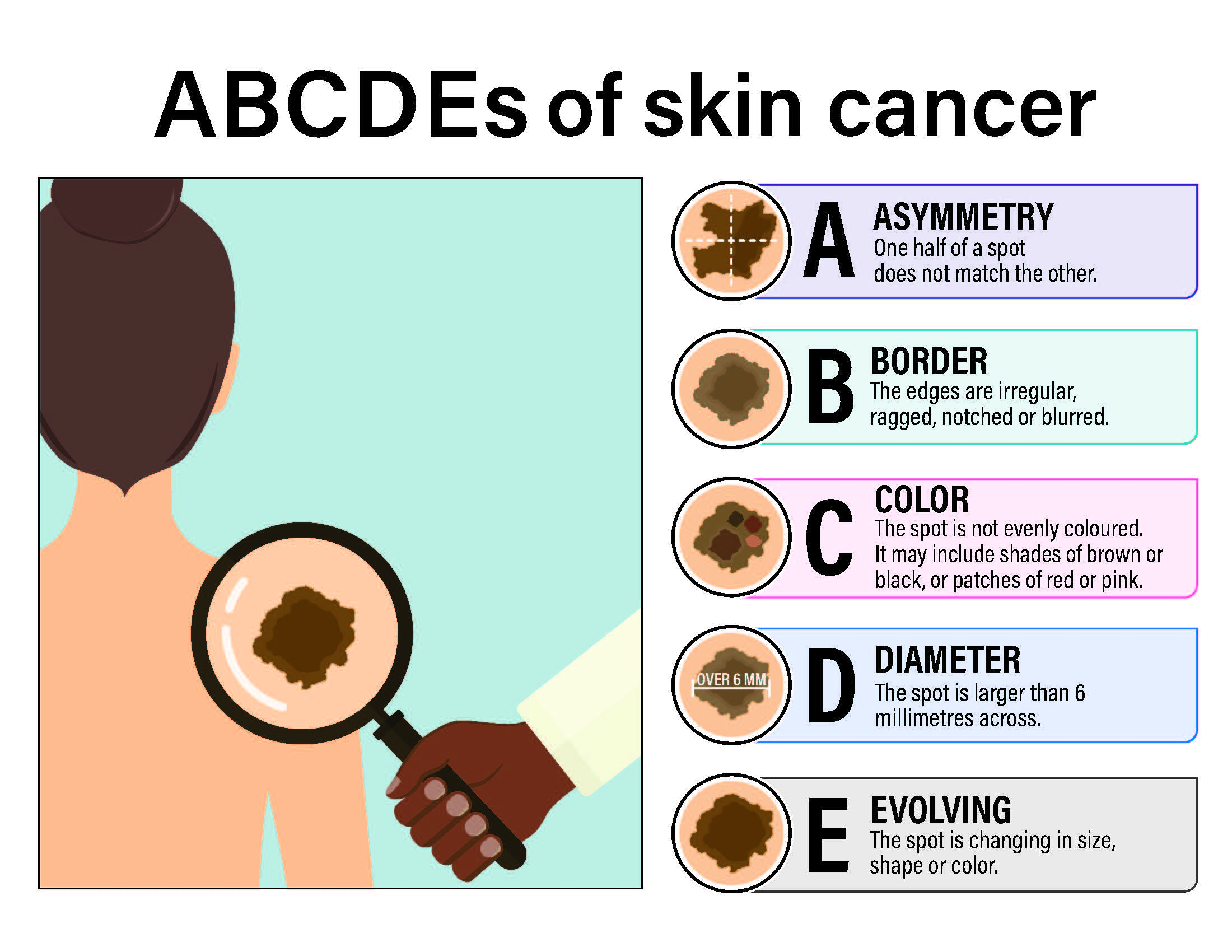
Hallmarks of skin cancer include the ABCDE signs: Asymmetry, Borders that are irregular, multiple Colors, Diameter of over 6 millimeter and Evolving or changing in size, shape or color:
If you have a personal or family history of melanoma and you are concerned about increased risk, consider talking to a healthcare provider about mutations in genes other than and that may increase your risk of melanoma.
Reference:
Narod, S.A., Metcalfe, K., Finch, A. et al. The risk of skin cancer in women who carry or mutations. Clinical Practice. 2024. 22(1): 7.
Disclosure: FORCE receives funding from industry sponsors, including companies that manufacture cancer drugs, tests and devices. All XRAYS articles are written independently of any sponsor and are reviewed by members of our Scientific Advisory Board prior to publication to assure scientific integrity.
Share your thoughts on this XRAY review by taking our brief survey.
posted 7/25/24
- What is my risk of developing melanoma?
- What type of skin cancer screening is recommended if I have an inherited or mutation?
- Does my family history influence my risk of developing skin cancer or melanoma?
- Should I see a ? If so, how often?
- How often should I follow up with a doctor regarding skin cancer screening recommendations?
The following resources can help you locate an expert near you:
Finding dermatologists
- The American Academy of Dermatology has a tool to find dermatologists by expertise, location or procedure.
- The Aim At Melanoma Foundation has a lookup tool for finding melanoma experts by location.
Related experts
If you learn that you are at high risk for melanoma, you may also need to see an ophthalmologist who can screen for melanoma in your eyes.
- The website for the American Academy of Ophthalmologists has a search feature to help you find an expert in your area.
Other ways to find experts
- Register for the FORCE Message Boards and post on the Find a Specialist board to connect with other people who share your situation.
- The National Cancer Institute (NCI)-Designated Comprehensive Cancer Centers have specialists who focus on prevention, screening and treatment for all types of cancer.
Updated: 09/22/2024